Top Links
Journal of Emergency Medicine and Care
ISSN: 2639-9253
The Effect of Cardiopulmonary Resuscitation Quality on Cardiac Arrest Outcome
Copyright: © 2020 Adel Hamed Elbaih. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Related article at Pubmed, Google Scholar
Background: Cardiac arrest is a leading cause of death in USA, nearly 90% of them fatal and Out of Hospital Cardiac Arrest (OHCA) is a leading cause of death worldwide. The Cardiopulmonary Resuscitation (CPR), especially if administered immediately after cardiac arrest, can double or triple a person’s chance of survival. CPR by training persons increases the frequency the survival rate. Therefore, we aim to look into the common pitfalls that both medical students and genior physicians face in the recognition and dealing Compression in Cardiopulmonary Resuscitation with its outcome.
Aims of the study: The Effect of Cardiopulmonary Resuscitation Quality on Cardiac Arrest Outcome in Adults
Targeted Population: All adult CA patients who are requiring urgent management in the ED, with Emergency Physicians for teaching high quality CPR protocol.
Targeted End User: Emergency Medicine, Critical Care Medicine and Anesthetist physicians
Methods: Collection of all possible available data about the Cardiopulmonary Resuscitation Quality on Cardiac Arrest Outcome by many research questions to achieve these aims so a midline literature search was performed with the keywords “critical care”, “emergency medicine”, “principals of Cardiac Arrest”, “High Quality Compression", " Cardiopulmonary Resuscitation”, “Automated External Defibrillator (AED)”. Literature search included an overview of recent definition, causes and recent therapeutic strategies in Cardiopulmonary Resuscitation.
Results: All studies introduced that the early diagnosis of Cardiopulmonary arrest and their interventions by simple tools e.g. HighQuality Compression and Automated External Defibrillator (AED) that face patients of critical care situations with increase survival rate.
Conclusion: High Quality CPR will be Improving Cardiac Resuscitation Outcomes both inside and outside the Hospital by; deeper chest compressions and rate of 85 to 100 compression per minute were also associated with higher survival rates.
Keywords: CPR; Emergency Medicine physicians; Cardiac arrest
Cardiac arrest is the loss of heart function in a person who may or may not have been diagnosed with heart disease. It can come on suddenly, or in the wake of other symptoms. Cardiac arrest is often fatal, if appropriate steps aren’t taken immediately [1].
Cardiac arrest may be caused by almost any known heart condition. Most cardiac arrests occur when a diseased heart’s electrical system malfunctions. This malfunction causes an abnormal heart rhythm such as ventricular tachycardia or ventricular fibrillation. Extreme slowing of the heart’s rhythm (bradycardia) also causes some cardiac arrests [2].
Other causes of cardiac arrest include:
• Scarring of the heart tissue
• A thickened heart muscle (cardiomyopathy)
• Heart medications
• Electrical abnormalities
• Blood vessel abnormalities
• Recreational drug use [3].
Cardiac arrest is a leading cause of death in US. There are more than 356,000 out-of-hospital cardiac arrests (OHCA) annually in the U.S., nearly 90% of them fatal, according to the American Heart Association’s newly released Heart and Stroke Statistics-2019 Update. According to the report, the incidence of EMS-assessed non-traumatic OHCA in people of any age is estimated to be 356,461, or nearly 1,000 people each day. Survival to hospital discharge after EMS-treated cardiac arrest is about 10% [4].
Out of hospital, cardiac arrest (OHCA) is a leading cause of death worldwide.
CPR combines rescue breathing, which provides oxygen for the lungs of the patient, and chest compression that keep the oxygenrich blood flowing until the heartbeat and breathing is normally restored. CPR requires proper training and knowledge before an individual due to the variation in adults, children and infants can practice it. CPR has proven to increase survival rate for the patient when given properly and immediately [5].
CPR, especially if administered immediately after cardiac arrest, can double or triple a person’s chance of survival. About 90 percent of people who experience an out-of-hospital cardiac arrest die [6].
Three million people in Sweden are trained in cardiopulmonary resuscitation (CPR). Whether this training increases the frequency of bystander CPR or the survival rate among persons, who have out-of-hospital cardiac arrests has been questioned. Methods We analyzed 30,381 out-of-hospital cardiac arrests witnessed in Sweden from January 1, 1990, through December 31, 2011, to determine whether CPR was performed before the arrival of emergency medical services (EMS) and whether early CPR was correlated with survival. RESULTS CPR was performed before the arrival of EMS in 15,512 cases (51.1%) and was not performed before the arrival of EMS in 14,869 cases (48.9%). The 30-day survival rate was 10.5% when CPR was performed before EMS arrival versus 4.0% when CPR was not performed before EMS arrival (P< 0.001) [7].
A recent study examined chest compression depth and survival in out-of-hospital cardiac arrest in adults and concluded that a depth of < 38 mm was associated with a decrease in ROSC and rates of survival [8].
So high quality Compression characters should be learned
➢ Place the heel of one hand in the center of the chest, Place other hand on top, Interlock fingers, Compress the chest, Rate 100- 120 min-1, Depth 5-6 cm, Equal compression: relaxation, RHYTHM of Compression and breath ratio 30:2, If there is more than one rescuer, the other should take over CPR, every 1-2 min to prevent provider fatigue and Ensure the minimum of interruption during the changeover to try continue cardiac output as physiological compensation to provide blood flow to vital organs so the role of physiologic monitoring such as specifically cardiac output, coronary and cerebral perfusion during resuscitation that may be sensitive to small changes that determine resuscitative efforts [8].
The defibrillation fact is the major predictor of outcome. it is a process in which an electronic device gives an electric shock to the heart. This helps re-establish normal contraction rhythms in a heart having dangerous arrhythmia or in cardiac arrest. in recent years’ small portable defibrillators have become available. These are called Automated External Defibrillators or AEDs. defibrillation is a process in which an electronic device gives an electric shock to the heart. This helps re-establish normal contraction rhythms in a heart having dangerous arrhythmia or in cardiac arrest. in recent years’ small portable defibrillators have become available. These are called Automated External Defibrillators or AEDs [7].
AEDs allow trained lay rescuers to successfully deliver defibrillation even before EMS can arrive. AEDs are safe, effective, lightweight, durable, low maintenance and easy to use. AEDs interpret heart rhythm and determine if a shock is required. The unit prompts the rescuer to deliver the shock, if necessary. An AED will NOT shock someone who does not need defibrillation [9].
Defibrillation is the only technique that is effective in returning a heart in VF or Pulseless VT to its normal rhythm. Although defibrillation is only one component of definitive care, it is probably the most important when it is provided rapidly and may be all that is necessary to save the victim’s life. Other life saving measures should not be minimized, but it is important to recognize the critically important role of rapid defibrillation in cardiac resuscitation Although defibrillation is only one component of definitive care, it is probably the most important when it is provided rapidly and may be all that is necessary to save the victim’s life. Other life saving measures should not be minimized, but it is important to recognize the critically important role of rapid defibrillation in cardiac resuscitation Lightweight and portable. Automatically analyze heart rhythms. Determine whether defibrillation is advised. Guide the user through defibrillation. Easy to use, safe, and effective. Long life batteries and comprehensive “self-checking” protocols [10].
Do not shock the patient if they are wet, dry off the torso, do not shock on a metal surface, do not touch the patient while they are being shocked. You can be shocked as well, remove any medication patches with a gloved hand and do not place pads over external defibrillator [11]. We aim to look into the common pitfalls that both medical students and genior physicians face in the recognition and dealing Compression in Cardiopulmonary Resuscitation with its outcome by the effect of cardiopulmonary resuscitation quality on cardiac arrest by increase the knowledge and skills on principals of basic life support for physicians, paramedical and medical students’ even popular people. As seen in Figure 1 the relation between high quality CPR, Defibrillation and early ACLS trained physicians which increase survival rate and improve outcome.
What is the Effect of Cardiopulmonary Resuscitation Quality on Cardiac Arrest Outcome in Adults (chest compression rateand depth)?
Evidence has accrued that cardiopulmonary resuscitation quality affects cardiac arrest outcome. However, the relative contributions of chest compression components (such as rate and depth) to successful resuscitation remain unclear.
This section includes Collection of all possible available data about the Cardiopulmonary Resuscitation by many research questions to achieve these aims so a midline literature search was performed with the keywords “critical care”, “emergency medicine”, “principals of Cardiopulmonary Resuscitation", "high quality CPR” and “AED”. Literature search included an overview of recent definition, causes and recent therapeutic strategies in Cardiopulmonary Resuscitation (CPR).
So the main aims and outcome of the study: initial assessment of Cardiopulmonary Arrest by simple tools to victim presentation e.g. Look, Listen Feels in less than 10 second with proper approach by High Quality Compression and Automated External Defibrillator (AED) that face patients of critical care situations with increase survival rate. And recognize potentially life-threatening conditions, reversible causes of cardiac arrest and to convey life-saving treatment so the key note here is that initial diagnosis in suspected arrest with initial treatment and rapid transfer proper cases to proper places.
While searching for this study, the Royal College of Emergency Medicine, Medline website and PubMed were searched for relevant the search was restricted to articles published between 1960 and 2011.
The databases were searched using the relevant terms, including all subheadings, and this was combined with a keyword search. Search words included “High Quality Compression”, “patients cardiac arrest” ‘reversible causes of cardiac arrest’, ‘cardiac arrest” and ‘resuscitation management. The search was also limited to humans and the English language. The National Library for Health and the National Guidelines Clearing House were also searched for relevant guidelines and reviews.
Review of “Quantifying the Effect of Cardiopulmonary Resuscitation Quality on Cardiac Arrest Outcome a Systematic Review and Meta-Analysis” and “Cardiopulmonary Resuscitation Quality: Improving Cardiac Resuscitation Outcomes Both Inside and Outside the Hospital”.
For “Quantifying the Effect of Cardiopulmonary Resuscitation Quality on Cardiac Arrest Outcome.” They searched for any clinical study assessing cardiopulmonary resuscitation performance on adult cardiac arrest patients in which survival was a reported outcome, either return of spontaneous circulation or survival to admission or discharge.
A 603 identified articles, 545 were excluded after review of the title and abstract. Forty-two studies were excluded for representing reviews (n=2), not assessing CPR quality metrics individually (n=22), comparing mechanical with manual CPR (n=2), reporting simulation data on manikins (n=1), including diseases other than cardiac arrest in the study population (n=2), not meeting outcome criteria (n=5), and representing overlapping publications from the same patient cohorts (n=8). A 6 additional studies excluded for assessing a categorical overall quality metric (e.g. “good” CPR versus “bad”) concomitant with associated survival. Final number of studies included in the systematic review is 10 [9].
Standardized quality scores for observational studies have not been established. Thus, quality assessment of the included studies was performed by evaluating and scoring 6 criteria on an integer scale (0 or 1, with 1 being better), including (1) study design, (2) multicenter or single-center designation, (3) assessment of CPR quality measures, (4) assessment of outcome, (5) evidence of bias, and (6) whether CPR quality assessment was a pre-specified aim. Studies with a sum from 0 to 4 were considered low quality, whereas those with a sum of 5 or 6 were considered high quality [10].
All included studies were either prospective cohort studies or post hoc analyses of primary clinical trial cohorts. Effect sizes were reported as mean differences. Standard errors were calculated using group SD or 95% CI measures. Survival outcomes were categorized as ROSC, survival to admission, or survival to hospital discharge [11].
Evidence for statistical heterogeneity between studies was tested by goodness of ft (χ2). Heterogeneity was also quantified with the I2 measure. This measure, ranging from 0% to 100%, represents the degree of inconsistency across studies included in the metaanalysis. Low, moderate, and high heterogeneity correspond to I2 values of 25%, 50%, and 75%, respectively [12].
CPR was performed by trained prehospital personnel such as emergency medical technicians and paramedics in 8 publications and by trained in hospital personnel such as nurses, physicians, and medical students in 3 publications. Study quality was high in 6 investigations, as defined by our scoring system [13].
For chest compression, depth six studies provided separate estimates for the relationship between chest compression depth and outcome. In 4 investigations, this outcome was ROSC; in 1 study, it was survival to hospital discharge; and in 1 study, it was survival to hospital admission. Cardiac arrest survivors were significantly more likely to receive deeper chest compressions than nonsurvivors (mean difference, 2.44 mm; 95% CI, 1.19–3.69; P< 0.001). No heterogeneity was detected among included studies [14].
For chest compression, rate six studies provided separate estimates for the relationship between chest compression rate and outcome. In 4 investigations, the outcome was ROSC; in 1 study, it was survival to hospital discharge; and in 1 study, it was survival to hospital admission. There was no overall difference in mean chest compression rate between survivors and no survivors (data not shown). We conducted a second analysis to determine whether proximity to a particular rate maximized survival (ie, that very high-compression rates were as detrimental as low rates). This was achieved by calculating the absolute difference between rates recorded among the 2 survival groups and a series of compression rate set points. For each such set point, the mean compression rate difference between survivors and non-survivors was assessed. Survivors were significantly more likely to receive chest compression rates closer to the range of 85 to 100 cpm, as shown in Figure 3 (absolute mean difference from 85 cpm, -4.81 cpm; 95% CI, -8.19 to -1.43 [P=0.005]; from 90 cpm, -6.58 cpm; 95% CI, -10.4 to -2.72 [P=0.001]; from 95 cpm, -6.58 cpm; 95% CI, -10.4 to -2.72 [P=0.001]; from 100 cpm, -5.04 cpm; 95% CI, -8.44 to -1.65 [P=0.004]). Low to moderate, non-statistically significant heterogeneity was detected among these associations [15].
This is the first systematic review and meta-analysis to evaluate such relationships including individual cardiac arrest events from an international and varied set of investigations. These results on the importance of chest compression depth are consistent with findings from previous laboratory studies such as a seminal investigation in dogs showing that cardiac output and blood flow were sensitive to compression depth. Another porcine study found that depth of chest compressions was closely related to the likelihood of ROSC. It is plausible that chest compression quality is more important during IHCA resuscitation in which defibrillation is less commonly required to achieve ROSC [16].
In the end of this study, they found CPR is an effective treatment modality for cardiac arrest and that the quality of CPR delivery is associated with survival. Specifically, we found that deeper chest compressions were associated with higher survival rates and that proximity to an ideal chest compression rate of 85 to 100 cpm was associated with improved survival in an independent fashion. Future efforts should be made to standardize how CPR quality variables are ascertained and reported to improve comparability between studies [17].
For “Cardiopulmonary Resuscitation Quality: Improving Cardiac Resuscitation Outcomes Both Inside and Outside the Hospital”. They include too much point but I will focus only on chest compression depth and rate. I will not mention how they did the Consensus Statement but I will take what related to my point. Therefore, for chest compression rate the 2010 AHA Guidelines for CPR and ECC recommend a chest compression rate of ≥100/min. As chest compression rates fall, a significant drop-off in ROSC occurs, and higher rates may reduce coronary blood flow and decrease the percentage of compressions that achieve target depth. Therefore, they suggest an optimum target of between 100 and 120 compressions per minute. For chest compression depth the 2010 AHA Guidelines for CPR and ECC, recommend a single minimum depth for compressions of ≥2 inches (50 mm) in adults [16,17].
We recommend increase knowledge and skills for the principals of CPR and other essential tools e.g. AED due to their simplicity of performance and reliability, even poor countries can use them in their systems and do so will prevent the collapse of healthcare services and improve patients' survival rates.
| Figure 1: Relation between CPR, Defibrillation and early ACLS trained physicians to outcome |
| Figure 2: Proper Approach to Cardiac Arrested Patient [2] |
| Figure 3: The Chain of Survival [3] |
Sequence |
Technical description |
Safety |
Make sure you, the victim and any bystanders are safe |
Response |
Check the victim for a response
If he responds leave him in the position in which you find him, provided there is no further danger; try to find out what is wrong with him and get help if needed; reassess him regularly |
Airway |
Open the airway
chin to open the airway |
Breathing |
Look, listen and feel for normal breathing for no more than 10 seconds |
Dial 997 |
Call an ambulance (997)
|
Send for AED |
Send someone to get an AED if available |
Circulation |
Start chest compressions
|
Give Rescue Breaths |
After 30 compressions open the airway again using head tilt and chin lift and give 2 rescue breaths
Continue with chest compressions and rescue breaths in a ratio of 30:2 |
If an AED Arrives |
Switch on the AED
If a shock is indicated, deliver shock
If no shock is indicated, continue CPR
|
Continue CPR |
Do not interrupt resuscitation until:
It is rare for CPR alone to restart the heart. Unless you are certain the person has recovered continue CPR |
Recovery Position |
If you are certain the victim is breathing normally but is still unresponsive, place in the recovery position
from the mouth
Be prepared to restart CPR immediately if the victim deteriorates or stops breathing normally |
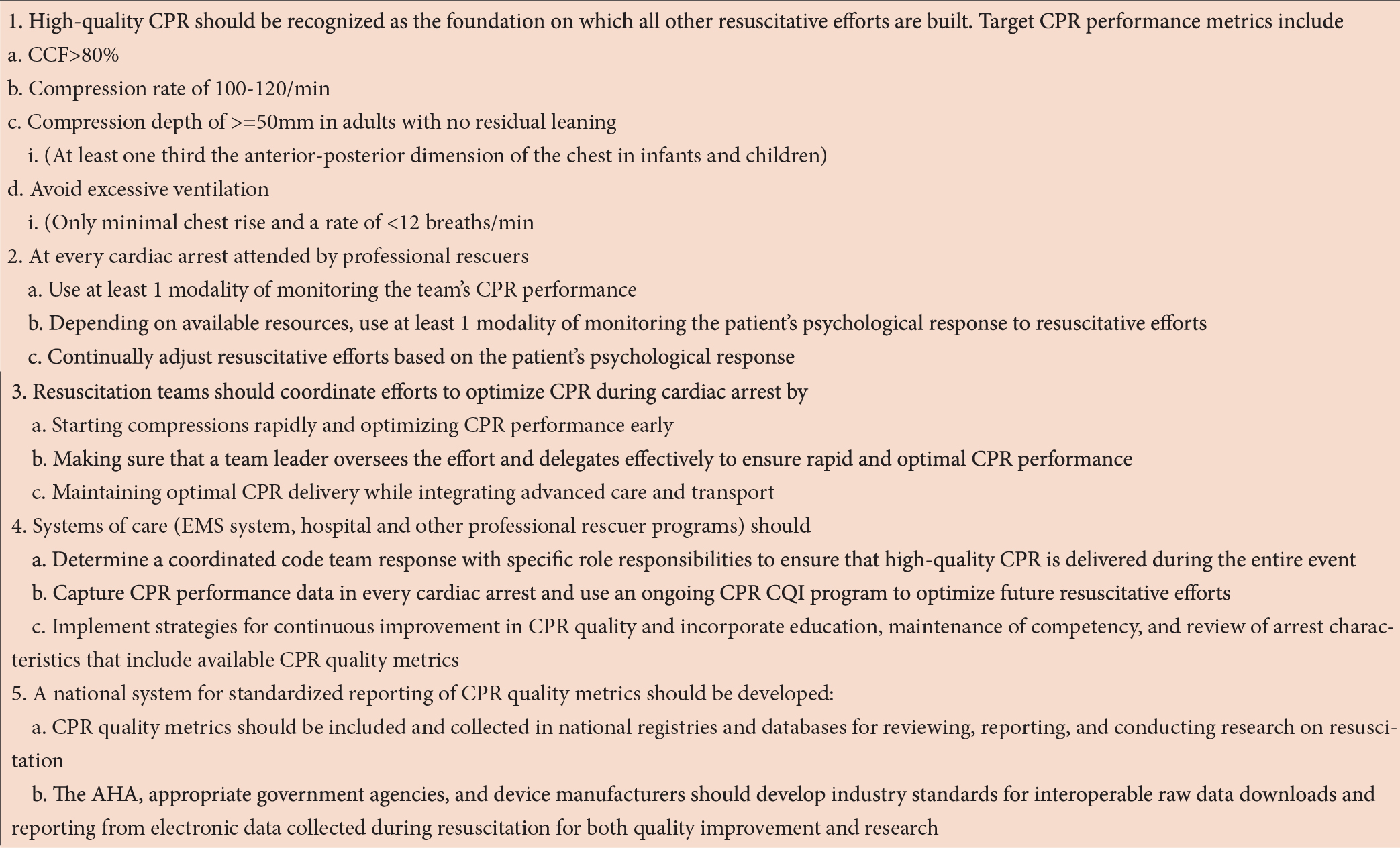 |
Table 2: Cardiac Arrest Evaluation Checklist [12]






































