Top Links
Clinical and Experimental Research in Cardiology
ISSN: 2394-6504
Cardio-Vascular Outcome Assessment of Dual Antiplatelet Therapy beyond 12 Months Following Drug Eluting Stent Implantation - Real World Scenario
Copyright: © Vijayakumar M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Related article at Pubmed, Google Scholar
Back ground and Rationale: In spite of recommendation for antiplatelet therapy following drug eluting stent (DES) implantation, the prescription for antiplatelet therapy in real world clinical practice varies from centre to centre as per physician discretion.
Objective: The study was intended to assess the cardiovascular outcomes and bleeding complications of dual antiplatelet therapy (DAPT) beyond 12 months following DES implantation.
Methodology: This is a single centre retrospective observation study conducted to assess the myocardial infarction, death, stent thrombosis, stroke, repeat revascularization and the bleeding in those received DAPT following DES implantation from Jan 2012 to Jan 2017. Data collection was done using electronic medical records. The choice of antiplatelet drugs, intensity and duration were under the discretion of physician.
Results: During the study period 3721 patients received DES and out of these 3118 patients were on DAPT beyond 12 months. The mean follow up period was 25.98months. The overall major adverse cardiac and cerebrovascular event (MACCE) was 4.1%. In this extended DAPT cohort the myocardial infarction occurred in 0.5%, stroke in 0.3% and 0.6% patients died. Only 0.2% stent thrombosis and repeat revascularization in 2.7% of patients were documented. Major bleeding occurred in 0.4%.
Conclusion and Relevance: Despite guide line recommendation DAPT beyond 12months following DES implantation significantly reduced the MACCE without increased risk of bleeding. There are no authorized guidelines for the long-term treatment of DAPT beyond 12 months in India.
Keywords: Drug Eluting Stent; Dual Antiplatelet Therapy; Stent Thrombosis; Bleeding; Stroke; Myocardial Infarction; Death
List of abbreviations: CAD: Coronary Artery Disease; PCI: Percutaneous Intervention; ACS: Acute Coronary Syndrome; DES: Drug Eluting Stent; DAPT: Dual Antiplatelet Therapy; MI: Myocardial Infarction; PTCA: Percutaneous Transluminal Coronary Angioplasty; MACCE: Major Adverse Cardiac and Cerebrovascular Event; TVR: Target Vessel Revascularization; ARC: Academic Research Consortium; PLATO: Platelet Inhibition and Patient Outcomes
Large number of patients with coronary artery disease (CAD) is undergoing percutaneous intervention (PCI) for many indications which includes stable CAD and acute coronary syndrome (ACS) refractory to medical management. Unless otherwise contraindicated almost all patients receives drug eluting stents (DES). Selection, initiation and continuation of dual antiplatelet therapy (DAPT) is as important as the interventional procedure for optimal outcome.
Even though there are recommendations from different medical organizations, to a large extent the practice of DAPT is influenced by operator discretion and the socioeconomic factors. The recommendation is to continue the DAPT for at least one year following the DES implantation. The newest DES with minimum strut thickness and non-permanent polymers may reduce the DAPT duration but as of now there are no recommendations.
Antiplatelet are drugs which inhibit the platelet aggregation and further blood clotting. This therapy prevents aberrant platelet activation in conditions like myocardial infarction (MI), ischemia and stroke [1].
Antiplatelet drugs form the backbone of cardiovascular drug therapy. As per guideline recommendation, the administration of DAPT consisting of aspirin and thienopyridine is for at least one year after coronary DES implantation [2]. There are mainly two pathways of platelet activation that is being interfered by DAPT: Aspirin inhibit cyclooxygenase mediated thromboxane A2 formation and inhibition of ADP activated surface receptor P2Y12 by thienopyridine derivatives like clopidogrel, ticagrelor, prasugrel, cangrelor [3].
The guideline made in past was based on studies carried out with first generation DES and less potent antiplatelet agents. Late stent thrombosis and inflammation due to the presence of permanent polymer was a concern. Newer second-generation DES utilize very recently developed anti anti-proliferative drugs like zotarolimus, everolimus and ridaforolimus are generally thinner, more biocompatible and may be coated with either permanent or bioabsorbable polymers [4]. Studies that compare these secondgeneration DES with first-generation DES propose that second -generation DES has been related with lesser risk of stent thrombosis. DAPT is also required with the 2nd generation stents, but optimal duration of use has not been firmly established.
The effectiveness of these P2Y12 antiplatelet drugs are proved in many clinical trials. InTRITON–TIMI-38 there was decreased rates of ischemic events associated with prasugrel therapy, whereas there was an increased risk of major bleeding. There were no major differences in the overall mortality between the treatment groups [5]. The superiority of ticagrelor over clopidogrel was established in PLATO double blind trial. Trial outcome shows that without an increase in the rate of overall major bleeding, there were decreased incidence of death from cardiac causes, stroke, or myocardial infarction [6].Prasugrel was tested against ticagrelor in ISAR-REACT 5 study and observed that patients who received prasugrel have considerably lower incidence of myocardial infarction, death or stroke than who received ticagrelor, and the incidence of major bleeding did not show major difference in between the two groups [7].
DAPT beyond 1 year after DES implantation, as compared with aspirin therapy alone, significantly decreased the risks of major adverse cardiovascular and cerebrovascular events including stent thrombosis whereas related with an increased risk of bleeding [8].
While offering freedom from cardiovascular events, the risk of bleeding is a concern in those continuing DAPT beyond 12 months. Our rationale for this study is to understand the outcome of those continuing DAPT beyond 12 months as the practice of DAPT prescription vary from patient to patient as decided by the treating physician.
This retrospective study on duration, intensity of DAPT following DES implantation and the cardiovascular outcome was conducted from September 2018-February 2019 from the department of adult cardiology. All patients who underwent Percutaneous Transluminal Coronary Angioplasty (PTCA) with DES eligible for DAPT were included in the study and the data collection process is shown in Figure 1. The study protocol was approved by Institutional Review Board at study center. The data of patients who received DAPT after PTCA was collected from electronic medical records. A total of 4,060 patients who underwent PTCA were screened for eligibility and among them 3,118 patients were chosen for this study. During the follow up, the following clinical events were analysedmyocardial infarction, stroke, death, stent thrombosis and repeat revascularization and the bleeding
A Major Adverse Cardiac and Cerebrovascular Event (MACCE) is defined as the composite of death, MI, stroke, stent thrombosis and target vessel revascularization (TVR) [9].
Definition of stent thrombosis as per Academic Research Consortium (ARC) was used to analyse stent thrombosis. Definite event (symptoms indicative of an acute coronary syndrome and angiographic or pathologic confirmation of stent thrombosis), probable event (death which is unexplained occur within 30 days or target vessel myocardial infarction without angiographic confirmation of stent thrombosis) possible event (any unexplained death after 30 days) [10].Myocardial infarction is described as a rise and drop of cardiac biomarkers jointly with evidence of myocardial ischemia with at least any one of the symptoms of ischemia: a) ECG changes suggestive of ischemia ST-T changes or new onset LBBB b) in ECG development of pathological q wave c) Imaging data of loss of viable myocardium or new regional wall motion deformity [11].
Ischemic stroke is a period of neurological dysfunction that is due to spinal, retinal or focal cerebral infarction. Intracerebral hemorrhage or hemorrhagic stroke is the fast developing clinical signs of neurological dysfunction imputable to a focal collection of blood inside the ventricular system or brain parenchyma which is not caused by trauma [12].
There are several definitions of bleeding in published trials and registries. Recent bleeding definitions consist of both laboratory parameters, such as drop in haemoglobin and hematocrit scores, and clinical events like the need for surgery or transfusion, hematomas, cardiac tamponade and varying degrees of bleeding [13]. Here in this study haemorrhagic events are classified according to bleeding definitions in Platelet Inhibition and Patient Outcomes(PLATO) trials. Target vessel revascularization is the unplanned repeat PCI or bypass graft placement for a stenosis in a different part of the vessel treated at the index PCI [14]
The collected data were documented in custom-made Microsoft excel sheet for further analysis. IBM SPSS version 20.0 software was used for performing statistical analysis. Frequency and percentage were used for expressing categorical variables. Continuous variables are expressed using mean and standard deviation.
Chi square test was used to test the statistical significance in the difference in the proportion of the categorical variable between groups. To test the statistical significance of the difference in the mean value of DAPT duration with respect to MACCE variables, Student’s t test was used for parametric data and Mann Whitney U test for non-parametric data.
In this retrospective study we have collected the data of 3118 patients who underwent DES implantation and continued DAPT beyond 12 months as per physician discretion. As in any other CAD studies, the male population was predominant here also with less than 20% females. More than half of them had 3 atherosclerotic risk factors and about7.6% were suffering from renal failure (Table 1).
Acute coronary syndrome (ACS) was the clinical presentation in majority of patients while stable angina was documented in 34% (Table 2).
Majority of patients had multivessel and multi lesion CAD, left anterior descending artery underwent revascularization with DES in 64% of cases. Sixty one percentages of patients received one stent and 891 patients were treated with 2 stents. While rest of patients received 3 or more stents .While short stents were used in 30.69% rest of them received long stents with 27.57% requiring very long stents of length more than 30 mm. Nearly one third of patients were given small diameter stents less than 2.5 mm diameter due to the small calibre vessel. The average stent length was 24.02mm and average stent length per person was 35.82mm (Table 3). Most of the stents used during this time period were second generation DES with few receiving first generation DES.
The initiation of DAPT therapy in these patients was as per physician discretion and the regime was as follows. With base line aspirin dose of 150 mg, 62.02 % received 75mg of clopidogrel, 33.86% received 90 mg of ticagrelor twice daily and 4.10% was given prasugrel. During the follow up period this initial dose and combination were changed as per physician discretion. In the follow up period, dose of aspirin reduced to 75mg along with clopidogrel 75mg (64.78% of patients), ticagrelor 90 mg (3.39% of patients) and prasugrel 10mg (13.28% of patients). Majority of them were on aspirin and clopidogrel probably due to availability and cost factor of ticagrelor. So 94% of patients on aspirin and ticagrelor where changed to aspirin and clopidogrel whereas 21.8% patients on aspirin and prasugrel also changed to aspirin and clopidogrel. Due to patient specific factors like age and weight of the patient, utilization of prasugrel was low and was only in 4.1% patients (Table 4).
During this follow up period MI including both NSTEMI and STEMI occurred in 16 patients. Out of 19 deaths, 6 were due to cardiac reasons. 10 patients developed ischemic stroke established by CT imaging. There was no haemorrhagic stroke. Out of 86 repeat revascularisation procedures 7 procedures were done for definite stent thrombosis. Out of 53 patients who developed bleeding episodes majority (38) were GI bleed. According to the PLATO bleeding category major bleeding occurred only in 11 patients (Table 5).
Many clinical studies evaluated the outcome of continuing DAPT beyond 12 months. DAPT prescription in real world clinical practice is beyond 12 months is a sole decision taken by the treating physician and the practice is well beyond the recommendation and clinical trial data. Situations like small calibre vessel PCI, long stents, overlapping stents, bifurcation, and LMCA interventions are few clinical situations where prolonged DAPT is chosen by physician. There was a vast difference in the intensity and duration of DAPT prescription among the consultants and hence we decided to look into the outcome of this practice.
In this study population 70% of patients received longer stents more than 20 mm and 27.5% had very long stents more than 30 mm. Small diameter stents were deployed in 28.3% and the average stented segment length per person was 35.82 mm .Significant number of patients (%) had ACS on presentation. All the above factors could be the reason for long duration DAPT in these patients.
Immediate post procedure 62.02% of patients received clopidogrel, 33.88%was given ticagrelor and 4.10% received prasugrel along with aspirin. In 62.02 % of patients on aspirin (150mg) and clopidogrel (75mg), 64.78% of them received aspirin 75mg and clopidogrel 75mg during their follow up period and 34.48 % patients continued with same initial dose of dual antiplatelet drugs and very few (0.72%) changed clopidogrel to ticagrelor. Only 0.8% among 33.86% patients on aspirin (150mg) and ticagrelor (90mg) continued same dual antiplatelets till their follow up period whereas 3.7% of them continued with same antiplatelet drugs but with low dose
aspirin (75mg). 95.35% patients initially on ticagrelor and aspirin changed their therapy from ticagrelor to either clopidogrel (94%) or prasugrel (1.4%) in their follow up period. During follow up period, in 128 patients (4.10%) who were initiated with aspirin (150mg) and prasugrel (10mg) after PCI, 81 of them continued with same therapy, 17 of them continued with same dual antiplatelet drugs but with reduced dose of aspirin (75mg) and in 30 patients prasugrel changed to either clopidogrel (21.8%) or ticagrelor (1.5%).
According to 2016 ACC/AHA guideline on DAPT duration in patients with CAD, Class I recommendation suggest duration of at least 6-12 months DAPT whereas Class II b recommendation which may be reasonable is made for prolonged DAPT beyond 6 to 12 months [15]. The proper optimal duration of treatment is unknown in patients who favour prolonged therapy.
As per European Society of Cardiology (ESC) guidelines based on 2017 ESC focused update on DAPT in CAD created in a joint effort with EACTS (European Association for Cardio-Thoracic Surgery), discussed that current evidence shows that there is a direct proportionality relation with the duration of DAPT both within and beyond 1 year of treatment and the risk of bleeding in these patients [16]. Also, proofs from studies suggest that risk of acute to very late stent thrombosis events have been lessen by DAPT. Also, extended DAPT beyond 1 year after PCI exerts the most of its advantage by decreasing the occurrence of spontaneous MI. Thus, optimal duration of DAPT following DES implantation is a balance between thrombotic and haemorrhagic events.
The mean DAPT duration in our study was 25.98 months. Our primary endpoint MACCE was found to be in 4.3% of patients which was relatable to 12 month or longer DAPT group (4.2%) in SMART-DATE trial study that assessed 6 month versus 12 month or longer DAPT in patients with ACS after PCI [17].
In PCI-CURE study it’s observed that there was reduction in rate of occurrence of MI in patients who received long term DAPT after PCI [18]. Out of 1355 patients of 12 month or longer DAPT group in SMART –DATE trial [17], 10 patients or 0.8 % developed MI whereas in our study 16(0.5%) patients in 3118 study subjects experienced MI. Also the study conducted by Eisenstein EL et al shows that extended use of clopidogrel reduced the risk of MI in patients with DES.21There is evidence from the results of the DAPT trial carried out by ACC indicating that extended duration of DAPT up to 30 months following index PCI with a DES results in lesser recurrent MIs (2.1% vs 4.1%) when compared with a12-month duration of DAPT and placebo [20].
Ischemic stroke developed in 0.3 % study subjects during our study period. This data is comparable with DAPT study by Mauri L et al comparing outcome in thienopyridine treated group (0.5%) and a placebo treated group [8].
Continued DAPT in all patients with different types of lesions was associated with reduced stent thrombosis as well. Studies done previously have shown that different stents [22,23] and thienopyridine derivative (P2Y12 inhibitors) were associated with varied rate of stent thrombosis (2.4% in clopidogrel group vs 1.1% in prasugrel group) [5]. In our study use of P2Y12 inhibitors beyond 12 months reduced risk of stent thrombosis (0.2%) despite of different types of antiplatelet drug or stent. The results of the DAPT trial carried out by ACC indicated that prolonged duration of DAPT up to 30 months following index PCI with a DES results in lesser stent thrombosis (0.4% in DAPT group vs 1.4% in placebo group)when compared with a12-month duration of DAPT and placebo [20].
One of the pooled analysis of different randomised trials by Jang JY et al identifies that when compared to standard duration of DAPT(≥12 months), target vessel revascularisation was increased in short duration DAPT [24]. Our study shows repeat revascularisation was required in (2.7%) of patients and which is well below the historical value.
Since prolonged antiplatelet therapy is related with increased bleeding risk, it is crucial to assess the risk against the potential benefit of antiplatelet therapy. In our study, the safety outcome is measured by the severity of bleeding which is assessed using PLATO definition. In this study population 0.4% of patients had minimal bleeding, 0.8% patients experienced minor bleeding, and 0.3% had other major type of bleed with a significant drop in haemoglobin (3-5g/dL) whereas 0.4% patients had major bleeding like intracranial bleeds.
A prospective observational study of ACS (stent) patients who received DAPT beyond 12 months by Beuno H et al showed that 2.1% of study population had clinically relevant bleeding. Among them 1.5% patients had bleeds requiring hospitalisation, 0.3% had bleeds with hemodynamic compromise, and 0.2% had intracranial bleeds [25].
In one of the retrospective study conducted by Howell SJ et al on the impact of long-term DAPT, the results revealed that about 23.8% of the patients experienced bleeding, out of which 0.2% had major type of bleeding [26]. In one of the previous study done by Costa F et al investigated the effects of ischemic (by PCI complexity) and bleeding risks on clinical outcomes and on the impact of DAPT duration after coronary stenting suggested that there was a consistent ischemic or mortality benefit from long term DAPT in the patients who are not at high risk of bleeding when compared with short-term DAPT regardless of the complexity of the intervention they underwent or the acute presentation at the time of PCI [27].
The estimated number of patients requiring DAPT following DES implantation is considerable and is increasing over time. The optimal duration of DAPT is uncertain and is limited to several years. The safety and efficacy of prolonged DAPT beyond one year is yet to be established in Indian population. The duration of DAPT should be determined assessing its benefit to risk scale. In our study we assessed the cardio protective nature of prolonged DAPT by estimating the incidence of MACCE outcomes as well as the risk nature of DAPT by observing the bleeding events.
Medication adherence of the patients was not assessed. Since it’s a retrospective study, there are under reported outcomes due to lost follow ups. Cause of death was not systematically recorded.
There are no similar studies done in Indian population.
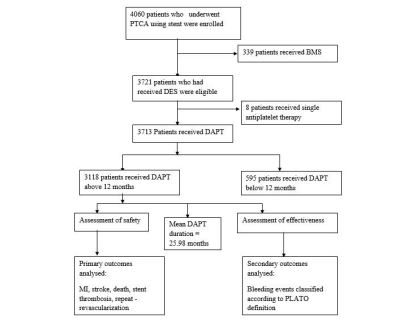 |
| Figure 1: Flow chart indicating data collection processes |
N =3118 |
|
Mean age (year) |
59.87±10.15 |
Male |
82.2% |
Female |
17.8% |
Diabetes Mellitus |
56.1 % |
Hypertension |
60% |
Dyslipidemia |
67.3% |
Renal failure |
7.6% |
Anaemia |
1.1% |
ACS |
2048 (65.7%) |
STEMI |
543 (26.51%) |
NSTEMI |
1349 (65.86%) |
Unstable angina |
156 (7.61%) |
Stable Angina |
1070 (34.3%) |
Vessel Involvement |
|
Single vessel |
1107 (35.5%) |
Double vessel |
1203 (38.6%) |
Triple vessel |
808 (25.9%) |
Location of Lesion |
|
Left anterior descending |
1997 (64%) |
Left circumflex |
1299 (41.7%) |
Right coronary artery |
1354 (43.4%) |
Stent distribution |
|
Single stent |
1907 (61.2%) |
Double stent |
891 (28.6%) |
Three or more |
320 (10.2%) |
Stent specifications |
|
Short stents (≥20mm) |
1427 (30.69%) |
Long stents(≥30mm) |
1282 (27.57%) |
Stent diameter ≤2.5mm |
1336 (28.73%) |
Average stent length |
24.02mm |
Average stent length per person |
35.82mm |
Number of patients on ASA 150mg+ clopidogrel 75mg (initiation therapy) |
1934 (62.02%) |
Number of patients on ASA 150 mg+ ticagrelor 90 mg (initial therapy) |
1056 (33.86%) |
Number of patients on ASA 150mg+ Prasugrel 10mg (initial therapy) |
128 (4.10%) |
During Followup Period |
|
Patients on ASA+ clopidogrel |
1934 |
Number of patients with ASA 75mg+clopidogrel 75mg (de-escalated dose) |
1253 (64.78%) |
Number of patients in which clopidogrel changed to ticagrelor |
14 (0.72%) |
Number of patients continued same dose of dual antiplatelets |
667 (34.48%) |
Patients on ASA+ ticagrelor |
1056 |
Number of patients with ASA 75mg+ ticagrelor 90 mg (de-escalated dose) |
40 (3.7%) |
Number of patients in which ticagrelor changed to clopidogrel and prasugrel |
992 (94%) and 15 (1.4%) respectively |
Number of patients continued same dose of dual antiplatelets |
9 (0.8%) |
Patients on ASA+ prasugrel |
128 |
Number of patients with ASA 75mg+ Prasugrel 10mg (de-escalated dose) |
17 (13.28%) |
Number of patients in which Prasugrel changed to clopidogrel and ticagrelor |
28 (21.8%) and 2 (1.5%) respectively |
Number of patients continued same dose of dual antiplatelets |
81 (63.2%) |
Primary outcome |
Secondary outcome |
||
MACCE: 4.3 % |
Bleeding: 1.7% |
||
Myocardial infarction |
16 (0.5%) |
GI Bleeding |
38 (1.2%) |
STEMI |
4 (0.1%) |
Intracranial |
4 (0.1%) |
NSTEMI |
12 (0.4%) |
Others |
11 (0.4%) |
Death |
19 (0.6%) |
PLATO Bleeding category |
|
Cardiac |
6 (31.6%) |
Minimal |
14 (0.4%) |
Non-cardiac |
13 (68.4%) |
Minor |
25 (0.8%) |
Stroke |
10 (0.3%) |
Other Major |
8 (0.3%) |
Ischemic |
10 (0.3%) |
Major |
11 (0.4%) |
Haemorrhagic |
0 (0%) |
|
|
Repeat revascularisation |
86 (2.7%) |
||
De novo lesion |
58 (1.8%) |
||
In stent Re-stenosis |
21 (0.7%) |
||
Stent thrombosis |
7 (0.2%) |
||






































