Top Links
Journal of Clinical and Experimental Genetics
Smoking and Male Infertility: A Comprehensive Review
Copyright: © 2023 Mahrukh Hameed zargar. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Related article at Pubmed, Google Scholar
Infertility is a serious concern affecting millions of couples globally. Natural conception is seen to be achieved in 80-85% couples leading 15 % couples suffer worldwide. Male factor is an important underlying cause associated with infertility. The debate that the ingredients’ of cigarette smoke negatively influence the masculinity attracts the scientific wit to look into the problem. To understand the link between smoking and male infertility, various attempts leading to contrasting results and conclusions have been made. Scientific studies confirm the impairment of fertility status in smoking men although few scientific reports from various studies negate the argument. Many studies have reported that the contents of cigarette smoke negatively affect sperm parameters. Research suggests that smoking has a role in increasing the reactive oxygen species (ROS) that leads to the oxidative stress. Increased oxidative stress impair the very characteristics of sperms structurally and functionally. This review work will precisely focus on the exposure of contents of the smoke in impairing the male fertility
Keywords: Male Infertility; Smoke; Reactive Oxygen Species; Sperm Parameters
Infertility is defined as a medical condition of inability of couples to conceive even after one year of frequent unprotected sexual intercourse. The debate that the ingredients of cigarette smoke negatively influence the sperm development in males attracts the scientific wit to look into the problem. well established research suggest that smoking has a role in increasing the reactive oxygen species (ROS) that leads to the oxidative stress .Increased oxidative stress impair the very characteristics of sperms structurally and functionally both. Sperm viability, sperm morphology, sperm motility are by and large affected due to rise in the oxidative stress which in turn affects the overall fertility status in males [1]. It is important to mention here that scientific studies have reached to contrasting conclusions. This review is an attempt to bring forward the relation between smoking and male infertility. Although this review paper will accommodate the arguable findings but the primary thrust will continue to explore the association between smoking and infertility besides bringing on to the surface the data on genetic and epigenetic lines also. Despite the cautions regarding the harm of smoking on the human health in general and reproductive wellbeing in particular from the Globally reputed health care institutions like WHO, smoking still continues to remain a worldwide phenomenon. WHO report confirmed 25% - 30% of men having an exposure to the smoking ingredients, Almost 40% of the men falling in the reproductive age smoke reports a study [2]. The findings based on survey by various organizations suggest the prevalence of male smokers increased from 721 million in early 80’s to 960 million in 2012. To understand the link between smoking and male infertility, various attempts leading to contrasting results and conclusions have been made. Scientific studies confirm the impairment of fertility status in smoking men although few scientific reports from various studies negate the argument [3]. The inconsistent and contrasting arguments are not surprising, there are possible and satisfying explanations for the varied results reported from various studies. Operations including varied assessment protocol and obscurity in comparing the data directly with smoking habit of the subject from heterogeneous risk factors plus the very mechanism that relates the smoking with the impaired fertility status can be the main reasons for contrasting arguments. This review work will precisely focus on the exposure of contents of the smoke in impairing the male fertility. To understand the broader look of the problem different shades of male infertility encompassing the physiological and pathological impression being impaired by the exposure to the smoke needs to be taken a comprehensive look of. The main thrust of this study will be to bring on to the surface the possible aspect of the role of smoking in the manifestation of genetic and epigenetic alternations in the male reproductive health. The review will further investigate the future scope of research to be carried out in meeting the demands of reproductive assistance. The establishment of negative implications of active or passive exposure to the cigarette on the health is a watchword advisory from the health experts. Researchers in general have recognized the bearings of cigarette smoking on the physiological and pathological state of human health be it cancer, chronic pulmonary disorders, cardio vascular ailments and the under discussion reproductive failures in both men and women. The data from various studies reveal that every year more than 8 million people die globally due to prolonged exposure to the cigarettes; with a figure of around 1.2 million of victims being passive smokers. Smoke from cigarrete comprises of gases, vaporized liquids, thousands of the compounds are released through the chemical process of hydrogenation, pyrolysis, oxidation, decarboxylation and dehydration. All this turn the cigarrete smoking one of the major causes of preventable morbidity and mortality. The relationship between cigarette smoking and infertility lacks large scale, population wide prospective studies [4].
Life style plays a very important role in determining the fertility status of males. Factors like smoking, extended exposure to high temperatures, insomnia, alcohol, age, drugs, obesity and extended exposure to electromagnetic radiation play a vital role in causing male infertility. Smoking heavily impacts the fertility status of men [5]. The available literature in the form of retrospective studies focuses on the effects of smoking on the sperm parameters. Experts on the basis of the scientific data usually caution men to abstain from smoking so as to improve the fecundity. Smoking not only affects the semen parameters, it may also reduce the success of assisted reproduction techniques (ART), such as in vitro fertilization (IVF) and intra cytoplasmic sperm injection (ICSI). Smoking has been suggested to contribute to decreased pregnancy rates through assisted reproductive procedures [6]. A study on couples undergoing ART demonstrated that couples in which the male partner recently smoked had a significantly lower live birth rate with IVF or ICSI (7.8% as against 21.1% in non-smoking males).Studies also reveal the significant increase in semen volume after smoking cessation. This might be an indication of the effect of smoking on accessory glands. Various studies have also reported the decrease in semen volume in smokers is inversely correlated to the number of cigarettes consumed daily [7].
In this review, we have reported that the contents of cigarette smoke negatively affect sperm parameters, seminal plasma, and various other fertility factors. Nevertheless, the actual effect of smoking on male fertility is the subject of further research. The effect of smoking on semen parameters is based on the well-established biological finding that smoking increases the presence of reactive oxygen species, thereby resulting in oxidative stress (OS). OS has devastating effects on sperm parameters, such as viability and morphology, and impairs sperm function, hence reducing male fertility. However, not all studies have come to the same conclusions. This review sheds light upon the association between smoking and male fertility and highlights the evidence that links smoking with male infertility.
The bibliographic databases PubMed and Google scholar were searched using the keywords like Male infertility and smoking, ROS and infertility. A total of 80 articles were identified discussing male infertility and smoking. 50 were selected for detailed reading, 34 articles with relevant study were incorporated in the study leaving 16 articles excluded from study.
Nicotine is proving to be the most harmful toxin, the presence of this lethal toxin in both serum and semen of smokers is reported from many studies. Studies confirm the positive correlation with the dose of smoking exposure. A metabolite of nicotine in the form of coitine is an alkaloid content associated with the tabacco. In some invitro studies, seminal cotinine and Trans-3- hydroxy cotinine levels were seen to be negatively associated to the motility status of sperms [8]. Some studies revealed the toxicological effects of nicotene to be dosage dependent. Nicotine concentration above 1mmol-1 was found to have serious bearings on both the viability and motility of the sperms. Another study by condorelli et al found that nicotine negatively impacts the progressive motility in a concentration dependent manner. In many studies nicotine and the metabolites associated with it were found to reduce the percentage of viability and motility [9]. A concentration of 100ng ml-1 of Nicotine was reported to promote the spermatozoa apoptosis, DNA fragmentation besides chromatin compactness [8].
The major intake route of cadmium in human body is associated with smoking. Cd possesses prolonged biological half-life of three to four decades in the human body which turns it into an accumulative toxin [9]. In many studies associated with human fertility among males, elevated levels of blood Cd and seminal Cd were observed in regular and second hand smokers. Various scientific studies reveal the reproductive toxicity due to exposure to the heavy metals [10].
Benzopyrene is another content associated with smoking. Benzopyrene is present in the Tar and is considered as a mutagen and carcinogen [11]. A study has shown the concentration of benzopyrene above 25 µg ml-1 negatively influences the percentage of acrosome formation.
Smoking has a negative impact on the sperm characteristics. A clinical study analyzed the sperms of 2542 healthy men between 1987 to 2004, the study revealed the lower semen volume, sperm count motility in smokers compared to non-smokers [12]. Study further suggested the dose dependent relationship between the sperm characteristics and exposure to smoking. A total of 19% reduction in the sperm concentration was seen in the males who smoked more than 20 cigarettes per day compared to the non-smoking controls [13].
In yet another study around 1786 men were screened for the possible association of smoking with male infertility [14]. Study by Kunzle et al showed the association of decreased number of sperms to the increased oxidative stress due to smoking. Studies have shown that toxin contents associated with tobacco smoking alter semen quality, semen density, Viability; Structure that leads to male infertility [15]. Tobacco smoking besides impairing the sperm characteristics is also a reason for upsurge DNA damage, aneuploidies. Studies also confirm the raised oxidative stress to an increased surge in the apoptosis of sperm atogenic cells [16]. The osmotic stress in the spermatozoa is a concern of the larger proportion of polyunsaturated fatty acids. Scientific studies also report the low proportion of scavenging enzymes in cytoplasm of the spermatozoa as a main reason of mild anti-oxidant capacity thereby affecting the overall defense mechanisms [17].
Due to the limited capacity for the recognition and repair of DNA damage spermatozoa are more prone to impairments; superoxide dismutase has been reported as a vital marker of male infertility [18]. The enzyme superoxide dismutase (SOD) shields the sperms from oxidative DNA damage (ODD), impaired motility and lipid peroxidation. The normal integrity and physiological functioning of the sperms is regulated by another enzyme, Glutathione peroxidase (GPX) as the enzyme is found to be proactive in the overall defense against the ROS [19].
A recent survey has shown approximately 120,000 young men in the reproductive age group from United Kingdom to be impotent due to the smoking related sperm impairments [20]. Although the studies pertaining to the effect of smoking on fertility status of men are debatable, the systematic investigation comparing sperm parameters between smokers and non-smokers can help in understanding the impact of smoking on the quality of the sperms in the infertilely males. Scientific studies have reported the reduction in the usual semen parameters like volume, motility, density, variability and normal morphology. Among all the sperm characteristics, sperm motility is important in determine the fertility status of males. Sperm creatinine kinase(CK) is an important reservoir for the regeneration of adenosine triphosphate and has an instrumental role in sperm motility [21]. As a key protein CK has an important role in the fertilization, smokers have been found to exhibit lower acrosin activity [22]. Zalata et al reported that the very activity of acrosin is impaired by the increased oxidative stress thereby indicating the possible underlying etiology associated with smoking. Many studies have confirmed the inhibitory role of tobacco smoking on protein associated with the capacitation of human spermatozoa. Changes in post translational modification due to exposure can be potentially the most possible cause linked to impaired sperm capacitation. Apart from having the negative impact on the semen quality, acrosin activity and protein phosphorylation, tobacco smoking impairs the other function of the spermatozoa like the expression of miRNAs and histone-- to-protamine transition [23].
Comprehensive scientific studies reveal that the consumption of tobacco causes sub-fertility by interfering in the synthesis of very essential reproductive hormones although some studies do generate a different opinion too [24]. A scientific survey carried on the infertile men reported the raised levels of both testosterone and androstenedione in smokers. Another survey divided the human subjects exposed to heavy, moderate and mild tabacco exposure and results with non-significant difference in the level of testosterone were reported. Since the testis are physiologically considered to be vulnerable to hypoxia amid the higher metabolic demand and relatively insufficient vascular supply through the spermatic cord [25]. Some researches successfully related the deficient oxygen delivery to the consumption of tobacco smoking thereby leading to the compromised state of hypoxia. Scientific studies confirm the detrimental effect of tar, benzopyrene on the overall testicular function [26].
Kunzle et al. [15] prospectively studied 2,105 participants in which 839 persons (39.9%) were smokers and 1,266 persons (60.1%) were non-smokers. Sperm concentration, motility, and morphology were significantly affected in smokers. In a large cross-sectional study involving the general healthy population, Ramlau-Hansen et al observed a significant reduction in sperm concentration, total sperm count and motility in smokers [27]. In a meta-analysis, Vine et al reported that the sperm concentration in smokers was approximately 13% lower than in non-smokers. Among normal healthy males, a 24% lower sperm concentration was observed in smokers in comparison to non-smokers [28]. A recent retrospective cross-sectional study of infertile couples compared 229 never-smokers, 56 past smokers, and 109 current smokers [29].
Lower testosterone levels were observed in both never-smokers and previous smokers than in current smokers. Other researchers have also found decreased testosterone levels in previous smokers [30]. In a study of the effect of smoking cessation on erectile dysfunction, Harte and Meston examined physiological and subjective sexual arousal indices during and after a smoking cessation program. The authors reported that smoking cessation considerably improved both physiological and self-reported indices of sexual health, irrespective of baseline erectile impairments [31].
Varicocele is an abnormal medical condition characterized by the enlargement of the venous plexus and is considered as one of the major causes for male infertility. Scientific studies has shown the incidence in smoking oligospermia patients ten times more than non-smokers. Almost 40 % of men suffer from infertility due to varicocele. Scientific studies also reveal the severe testicular hypoxia, venous stasis, reflux of toxic metabolites, and hormonal dysfunctioning in smoking patients than in the non-smokers [32].
Smoking causes the surge in the overall oxidative stress has long been noticed by researchers. Kiziler et al. found the raised concentration of malondialdehyde and protein carbonyls in smoking male infertile patients. Both the compounds are the indicators of higher reactive oxygen species (ROS) generated either by endogenous or exogenous means [33]. The endogenous cause can be the macrophage, immature spermatozoa while exogenous generation of ROS include smoking, alcohol or industrial toxins.
Assisted reproductive technology (ART) is an important tool in the hands of fertility experts. The exact reason that brings on to the surface the mechanism that exerts the detrimental effect of cigarette smoking on the output of ART are not known. The effect of smoking on ART results has been considered as an important problem to work on. Studies by zitzmann et al related male smoking with lower rates of success in about 148 patients seeking IVF [34]. Another study confirmed that the men with more than five years of smoking exposure have relatively higher risk of multiple births while undergoing IVF or GIFT. Studies also confirm the passive effect of smoking in female oocyte retrieval. Few studies mention a decrease of oocyte retrieval by 46 % in females where respective male partner is exposed to smoking. One faces the difficulties in relating the impact of smoking on the outcome of ART due to the cyclic nature of ART [35].
A series of studies related to smoking and male infertility suggest that the DNA damage potentially impairs the oocyte fertilization and the embryonic development thereby leading to the infertility. Studies suggest the increase in the percentage of fragmented or damaged DNA in the spermatozoa of male smokers [36]. In male smokers the fragmented DNA was found to be increased by 4.7 % in comparison to 1.1 % in nonsmokers. Detrimental effect of tobacco smoking altering the motility precisely the swim up selection of the sperms has been reported in various studies [37]. Some studies have linked the increased risk of aneuploidy to the smoking. Recent researches in this field have demonstrated the considerable difference of 1.7 folds between smokers and non-smokers. Many studies reveal the negative co-relation between the DNA damage and the sperm count and sperm motility in the infertile males.
By stimulating the hypothalamic-pituitary axis, nicotine can impair the release of growth hormone, vasopressin and oxytocin which in turn inhabit the lutienizing hormone levels LH and prolactin. Studies reveal the raised levels of LH and FSH in smokers, prolactin levels were seen lower in smokers than in non-smokers reports a study by ochedalski et al [38]. Some studies report the lydig cell failure in smokers due the interference of elements of tobacco. Some studies have shown the contradictory results regarding the influence of smoking on the products of HPG axis mainly the androgens. A study investigating 889 fertile men with mild, moderate and heavy exposure to smoking mentioned no significant differences in FSH, LH or testosterone levels [39].
This review is an attempt to bring the possible effects of smoking and elements of smoking on the overall status of male fertility. Although scientific literature has contradictory say on the impact of smoking on male fertility, however the measurable effects of smoking on the quality and functioning of sperms too can’t be denied and many studies have successfully related the severity of sperm disorder with both active and passive smoking. Researchers, clinicians must aware the infertile men about the possibilities of successful conception due to the smoke cessation. The available data to attribute the infertility in men to the elements of smoking must be taken a serious note before counseling the patients at clinics providing assistance to the childless couples.
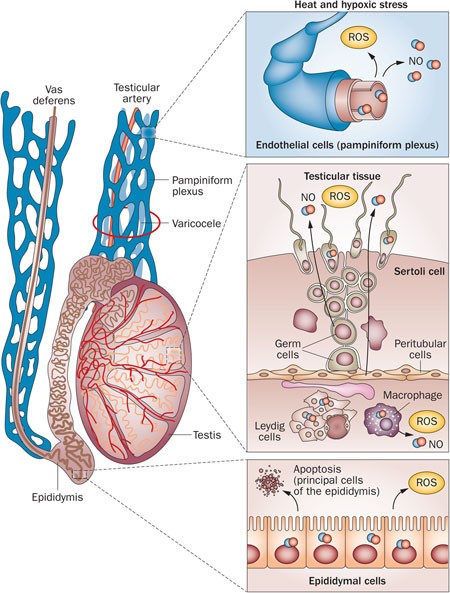 |
| Figure 1: smoking and viracocele Image adopted from Agarwal A, Hamada A & Esteves S. Insight into oxidative stress in varicocele-associated male infertility: part 1. Nat Rev Urol 9, 678-690 (2012). https://doi.org/10.1038/nrurol.2012.197 |
 |
| Figure 2: Smoking and DNA Damage, Image Adopted from Toor JS & Sikka SC (2019) Human spermatozoa and interactions with oxidative stress. In Oxidants, Antioxidants and Impact of the Oxidative Status in Male Reproduction (pp. 45-53). |






































